DID YOU KNOW?
• Around 85 percent of CDCR’s releasing population are eligible for Medi-Cal.
• California is the first state in the nation to provide Medi-Cal funded pre-release services to people in prison.
• CalAIM helps people continue vital mental health and substance use disorder treatment services after release.
• CalAIM is operational at all 31 California prisons.
• CalAIM links released patients to timely and vital Medi-Cal-covered health care services as well as provider reimbursement payments for covered expenses.
A Smoother Transition To The Community
California Department of Corrections and Rehabilitation (CDCR), California Correctional Health Care Services (CCHCS), and in partnership with the Department of Health Care Services (DHCS) are proud to announce the launch of the California Advancing and Innovating Medi-Cal (CalAIM) Justice-Involved Reentry Initiative within the state’s prison system.
California is the first state in the nation to enable its prison system to function as a state-sponsored health coverage billing entity for pre-release services. This groundbreaking effort ensures that thousands of incarcerated individuals with chronic health conditions, mental health needs, or substance use disorders receive linkages to the critical care and supportive services they need through Medi-Cal as they transition back to their communities.
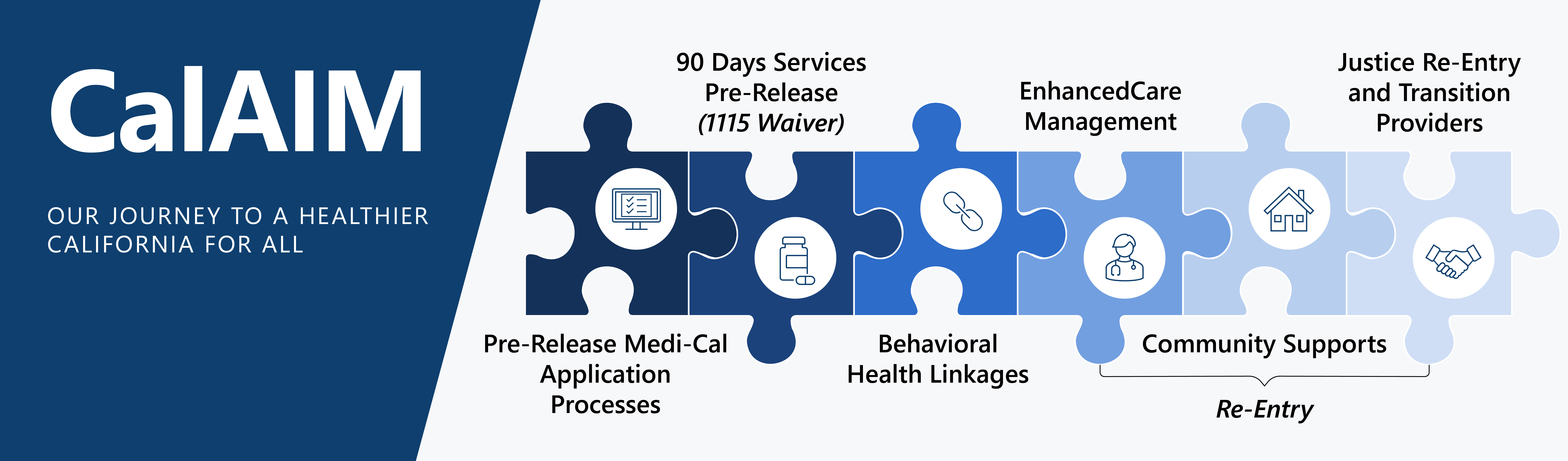
The CalAIM Justice-Involved Reentry Initiative focuses on:
-
- Enhancing the Medi-Cal Application Process: Submitting applications 135 days before release and activating pre-release services benefits 90 days prior to release.
- Pre-Release Services: Assignment to a Managed Care Plan, if needed; development of a Reentry Care Plan; Enhanced Care Management Services to include connecting to community lead care managers to assist with linkages to providers for critical care and supportive services; and a warm hand off between the incarcerated person and their lead care manager.
Population Education Materials
What Is CalAIM?
The CalAIM Justice-Involved Reentry Initiative helps people stay healthy when they leave prison. It allows eligible Californians to sign up for Medi-Cal (a health insurance program) before they are released. This way, they can keep getting the care they need after they enter the
community.
It also helps them get medicine, medical equipment, and other support for this important transition.
What services are included as part of CalAIM?
-
-
-
- Help signing up for Medi-Cal (if eligible)
- Pre-release planning
- Support from Lead Care Managers for health care, transportation, food, clothing, and other community resources
- Mental health and substance use treatment services
-
-
Who is a Lead Care Manager?
A Lead Care Manager is someone in the community who helps create a Reentry Care Plan for a soon-to-be-released incarcerated person’s needs, like doctor visits and mental health care. They help guide and support with addressing health and social needs.
What is a Reentry Care Plan?
A list of services that describes your reentry needs. These needs may include your health care appointments, food, clothing, and support groups. You will work with your prerelease coordinator to create your Reentry Care Plan. The plan will be given to your Lead Care Manager who will reach out to you after release.
Still have questions?
For questions about CalAIM, please contact Lifeline@cdcr.ca.gov.
What is Medi-Cal?
It helps pay for medical care for eligible California residents. Medi-Cal eligibility depends on income, age, and health conditions. A benefit worker will reach out to assist an incarcerated person with their application. For more information about Medi-Cal, visit: https://www.dhcs.ca.gov/Pages/myMedi-Cal.aspx
What is a Pre-Release Care Coordination Team?
The team that works in institutions to help set up post-release health care needs and connect incarcerated people with a Lead Care Manager
What is a Managed Care Plan?
A type of health insurance that organizes your care through a group of doctors and services. Kaiser Permanente, Blue Shield, Anthem Blue Cross, and Health Net are some examples of Managed Care Plans.
More CalAIM facts
- The California Advancing and Innovating Medi-Cal (CalAIM) Justice-Involved Reentry Initiative is jointly managed by The California Department of Corrections and Rehabilitation (CDCR), California Correctional Health Care Services (CCHCS), and the Department of Health Care Services (DHCS).
- This helps incarcerated individuals with chronic health conditions receive linkages to the critical care and support they need as they transition back to their communities.
- CalAIM helps people submit their Medi-Cal applications 135 days before release, activating pre-release services benefits 90 days prior to release.
- Mental health and substance use disorder treatment services are critical for someone transitioning to the community, and CalAIM helps people continue their treatment after release.
- All this planning helps for more than health care. CalAIM also helps plan for transportation, housing, food, clothing and other community resources.
- CalAIM was launched Feb. 3 and provided 450 reimbursement payments in the first week alone.
- Operations were set in place after a small preliminary cohort spread across three institutions – California Health Care Facility (CHCF), California Medical Facility (CMF), and Central California Women’s Facility (CCWF), which demonstrated the efficacy of Enhanced Care Management Services and pre-release planning.
- Best practices for CalAIM were also developed through collaboration with stakeholders, refining the approach for broader application to all 31 prisons statewide.
- CalAIM was launched in a phased approach. Phase 1, which began Feb. 3, included stakeholder/patient notifications, initiated identification and evaluation of CDCR’s incarcerated population for eligibility and allowed reimbursement of medication claims.
- Phase 2 of CalAIM began in April, and included reimbursement of Care Management claims, claim validation, claim receipt, and claim resubmission.
- Phase 3 will allow for service billing for reimbursement of additional services provided within 90 days of release including Physical and Behavioral Health consultations, medications, durable medical equipment and, laboratory and radiology services.
