California Department of Corrections and Rehabilitation (CDCR), California Correctional Health Care Services (CCHCS), and in partnership with the Department of Health Care Services (DHCS) are proud to announce the launch of the California Advancing and Innovating Medi-Cal (CalAIM) Justice-Involved Reentry Initiative within the state’s prison system.
California is the first state in the nation to enable its prison system to function as a state-sponsored health coverage billing entity for pre-release services. This groundbreaking effort ensures that thousands of incarcerated individuals with chronic health conditions, mental health needs, or substance use disorders receive linkages to the critical care and supportive services they need through Medi-Cal as they transition back to their communities.
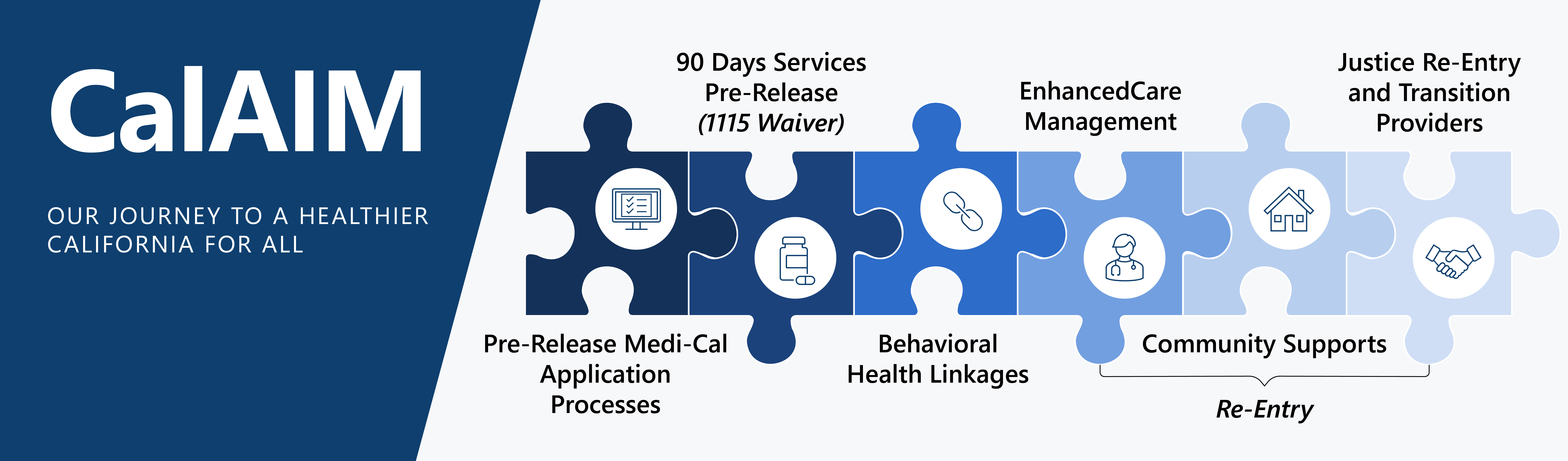
The CalAIM Justice-Involved Reentry Initiative focuses on:
-
- Enhancing the Medi-Cal Application Process: Submitting applications 135 days before release and activating pre-release services benefits 90 days prior to release.
- Pre-Release Services: Assignment to a Managed Care Plan, if needed; development of a Reentry Care Plan; Enhanced Care Management Services to include connecting to community lead care managers to assist with linkages to providers for critical care and supportive services; and a warm hand off between the incarcerated person and their community lead care manager.
Population Education Materials
What Is CalAIM?
It’s an initiative that helps incarcerated individuals get ready to return to the community. CalAIM will help enroll them for health care coverage and additional support through Medi-Cal, if eligible.
What is Medi-Cal?
It helps pay for medical care for eligible California residents. For more information about Medi-Cal, visit: https://www.dhcs.ca.gov/Pages/myMedi-Cal.aspx
Who can receive CalAIM and Medi-Cal?
Medi-Cal eligibility depends on income, age, health conditions. Patients may qualify if they have certain health needs, like a mental health issue, substance use disorder, a long-term or serious health condition, brain injury, HIV or AIDS, or are pregnant or recently had a baby. They can begin applying for Medi-Cal benefits 6 months before their release date. A benefit worker will reach out to assist you with the application.
What services are included as part of CalAIM?
-
-
-
- Help signing up for Medi-Cal (if eligible)
- Pre-release planning
- Support from Community Lead Care Managers for health care, transportation, food, clothing, housing, and other community resources
- Mental health and substance use treatment services
-
-
What If someone doesn’t qualify for Medi-Cal benefits?
A CDCR/CCHCS Pre-Release Coordinator will still help by connecting the individual with community services and providing resources, medications and contacts.
Still have questions?
For questions about CalAIM, please contact Lifeline@cdcr.ca.gov.
